
Retina Glossary PDF: Comprehensive Guide
Embark on a visual journey with our comprehensive retina glossary. This guide unravels complex ophthalmic terms. It offers clarity on retinal structures, conditions, and diagnostic procedures. Enhance your understanding of eye health and vision. Learn essential terminology for optimal eye care.
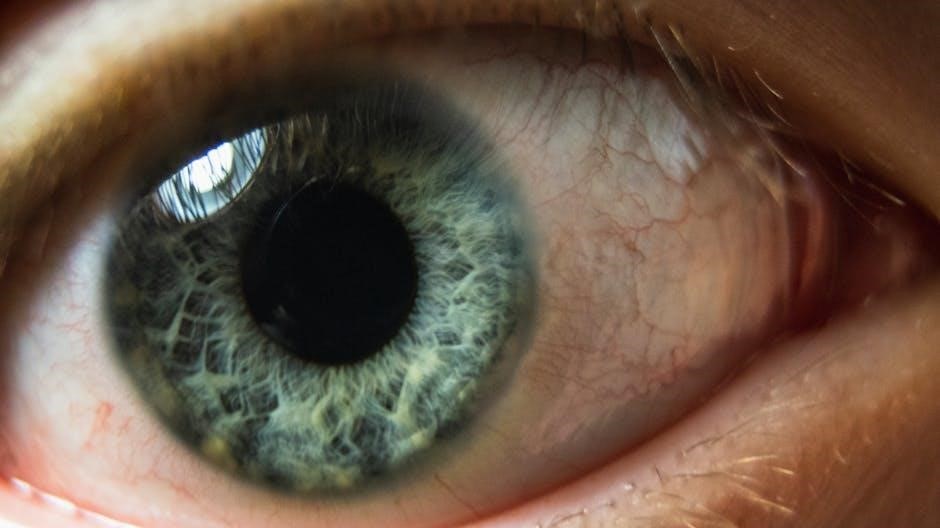
The retina, a delicate layer of tissue, lines the inner eye. It plays a vital role in vision. Like film in a camera, it captures images projected through the lens. The retina converts light into electrical signals. These signals travel to the brain via the optic nerve. This process allows us to see the world around us.
Understanding the retina is crucial for maintaining eye health. This glossary provides definitions of key retinal terms. It covers structures like the macula and fovea. It also explains conditions like macular edema and retinal detachment. Diagnostic terms, such as refraction, are also included.

The retina’s intricate structure includes rods and cones. Rods help us see in low light. Cones enable color vision and visual acuity. The macula, with the fovea, is responsible for sharp, central vision; Damage to the retina can lead to vision impairment. Early detection and treatment are essential.
This glossary aims to empower you with knowledge. Learn about your eyes and vision. Understand common retinal conditions. Make informed decisions about your eye care.
Retina: Definition and Function
The retina is the innermost layer of the eye. It’s a thin, light-sensitive tissue. It lines the back wall of the eye. Think of it as the film in a camera. The retina receives images projected through the lens.
Its primary function is to convert light into neural signals. These signals are then sent to the brain. This allows us to perceive the world visually. The retina contains photoreceptor cells called rods and cones. Rods are responsible for vision in low light conditions. Cones are responsible for color vision and visual acuity.
The retina is a complex structure. It comprises multiple layers of neurons. These layers work together to process visual information. The optic nerve connects the retina to the brain. It transmits these processed signals.
Damage to the retina can result in impaired vision. Various conditions can affect the retina. These include macular degeneration, retinal detachment, and diabetic retinopathy. Understanding the retina’s structure and function is essential. It helps in diagnosing and treating these conditions. This glossary provides key terms related to the retina. It aids in understanding its role in vision.
Key Retinal Structures
The retina is comprised of several key structures. Each plays a vital role in vision. Understanding these structures is crucial for comprehending retinal function and related conditions. The photoreceptor layer contains rods and cones. Rods enable vision in low light, while cones facilitate color vision and acuity.
The macula is a small, specialized area of the retina. It is responsible for central, high-resolution vision. Within the macula lies the fovea, a pit-like depression. It contains the highest concentration of cones. This area provides the sharpest vision.
The optic disc is where the optic nerve exits the eye. It creates a blind spot because it lacks photoreceptors. Blood vessels that supply the retina also enter and exit through the optic disc.
The retinal pigment epithelium (RPE) is a layer of cells. It supports the photoreceptors. It also absorbs stray light to prevent scattering. The inner limiting membrane is the innermost boundary of the retina.
These structures work together to capture light. They convert it into neural signals. They transmit these signals to the brain. Damage or dysfunction in any of these structures can lead to vision impairment. Understanding these key components is essential for diagnosing and managing retinal diseases.
Macula and Fovea: Centers of Vision
The macula and fovea are critical components of the retina. They are essential for central vision. The macula, located in the central retina, is responsible for sharp, detailed vision. This allows us to read, recognize faces, and perform tasks requiring visual precision. Within the macula lies the fovea, a small depression packed with cone photoreceptors.
The fovea is the area of highest visual acuity. Its high concentration of cones enables us to see fine details and colors clearly. Light focuses directly onto the fovea. This maximizes visual clarity. The macula and fovea work together to provide the central vision. This is crucial for daily activities.
Conditions affecting the macula, such as macular degeneration, can severely impair vision. These conditions often lead to difficulty with reading and recognizing faces. Understanding the structure and function of the macula and fovea is important.
The macula is essential to process straight-ahead vision and color vision. The fovea contributes to maximum acuity of vision. Maintaining the health of these regions is vital for preserving visual function. Regular eye exams can help detect and manage macular problems early.
Optic Nerve: Connecting the Eye to the Brain
The optic nerve serves as the vital link between the eye and the brain. It transmits visual information gathered by the retina to the brain for processing. This neural cable extends from the back of the eye to the brain. It carries signals that enable us to perceive images, colors, and movement.
The optic nerve is composed of millions of nerve fibers. They transmit electrical impulses generated by the retina’s photoreceptor cells. These impulses travel along the optic nerve to the visual cortex in the brain. Here they are interpreted as visual information.
The optic nerve head, also known as the optic disc, can be visualized during an eye exam. Examination of the optic nerve can reveal signs of eye disease. Conditions such as glaucoma can damage the optic nerve, leading to vision loss.
The optic nerve is crucial for sight. Damage or disease affecting the optic nerve can result in impaired vision or blindness. Regular eye exams are essential. They monitor the health of the optic nerve. This ensures early detection and management of potential problems, preserving visual function. The optic nerve is an important part of the visual pathway.
Common Retinal Conditions
The retina, a delicate tissue lining the back of the eye, is susceptible to various conditions that can impair vision. Macular degeneration, a prevalent age-related disease, affects the macula, leading to central vision loss. Diabetic retinopathy, a complication of diabetes, damages blood vessels in the retina, causing vision impairment.
Retinal detachment occurs when the retina separates from the underlying tissue, requiring prompt medical attention to prevent permanent vision loss. Macular edema involves swelling in the macula, resulting in blurred or distorted vision. Epiretinal membrane formation on the retina can cause visual distortions and decreased vision.
Retinal macroaneurysms, dilations of retinal vessels, can lead to bleeding and vision problems. These conditions highlight the importance of regular eye exams for early detection and management. Early intervention can help preserve vision and prevent further damage to the retina.
Understanding these common retinal conditions is crucial for maintaining optimal eye health. Awareness of symptoms and risk factors can facilitate timely diagnosis and treatment. Consult with an eye care professional for comprehensive evaluations and personalized management plans to protect your vision.
Macular Edema: Swelling in the Macula
Macular edema is a condition characterized by swelling in the macula, the central part of the retina responsible for sharp, detailed vision. This swelling occurs due to fluid accumulation in the macula’s layers, disrupting its normal function. Macular edema can result from various underlying causes, including diabetic retinopathy, retinal vein occlusion, and inflammation.
Symptoms of macular edema include blurred vision, distorted vision, and decreased color vision. Individuals may experience difficulty with reading, recognizing faces, and performing tasks that require fine visual acuity. The severity of symptoms can vary depending on the extent of swelling and the underlying cause.

Diagnosis of macular edema typically involves a comprehensive eye exam, including optical coherence tomography (OCT) to assess the macula’s structure and thickness. Treatment options aim to reduce swelling and improve vision. These may include anti-VEGF injections, laser therapy, or corticosteroids.
Early detection and prompt treatment are crucial for managing macular edema and preventing permanent vision loss. Regular eye exams, especially for individuals with risk factors such as diabetes, can help identify macular edema in its early stages. Proper management can help preserve visual function and improve quality of life.
Retinal Detachment: Separation of the Retina
Retinal detachment refers to the separation of the neurosensory retina from the retinal pigment epithelium (RPE). The retina, a light-sensitive layer at the back of the eye, relies on the RPE for support and nourishment. When these layers separate, the retina loses its blood supply, leading to vision impairment.
Symptoms of retinal detachment may include sudden flashes of light (photopsia), floaters, a shadow or curtain in the field of vision, and blurred vision. These symptoms can occur gradually or suddenly and should be promptly evaluated by an eye care professional.
Retinal detachment can be caused by various factors, including retinal tears or holes, trauma, inflammation, and underlying eye conditions. Risk factors include aging, nearsightedness (myopia), previous eye surgery, and a family history of retinal detachment.
Diagnosis involves a comprehensive eye examination, including dilated fundus examination to visualize the retina. Treatment typically requires surgical intervention to reattach the retina. Surgical options include pneumatic retinopexy, scleral buckling, and vitrectomy. Early diagnosis and treatment are crucial to prevent permanent vision loss. Regular eye exams, especially for individuals at risk, can help detect retinal detachment early and ensure timely intervention.
Epiretinal Membrane: Formation on the Retina
An epiretinal membrane (ERM), also known as a macular pucker or cellophane maculopathy, is a thin, semi-transparent membrane that forms on the inner surface of the retina. This membrane typically develops over the macula, the central part of the retina responsible for sharp, detailed vision.
The formation of an ERM is often related to age-related changes in the vitreous humor, the gel-like substance that fills the eye. As the vitreous shrinks, it can pull on the retina, causing cells to migrate and proliferate on the retinal surface, forming the membrane.
Symptoms of an ERM can vary depending on its size and location. Some individuals may experience mild distortion or blurring of vision, while others may have more significant visual disturbances, such as difficulty reading or seeing fine details. In some cases, an ERM may be asymptomatic and discovered during a routine eye exam.
Diagnosis of an ERM is typically made through a comprehensive eye examination, including optical coherence tomography (OCT), which provides detailed images of the retina. Treatment is usually not necessary for mild cases with minimal symptoms. However, if the ERM significantly affects vision, a vitrectomy surgery may be recommended to remove the membrane and improve visual acuity. Early detection and monitoring are essential to manage ERMs effectively and prevent potential vision loss.
Retinal Macroaneurysm: Dilation of Retinal Vessels
A retinal macroaneurysm (RAM) is a localized dilation or bulging of a retinal artery, typically occurring in older individuals with hypertension or other cardiovascular conditions. These aneurysms can develop due to weakening of the arterial wall, leading to expansion and potential rupture.
RAMs are often found near arteriovenous crossings or branch points in the retinal vasculature. They can manifest as small, round or oval lesions, sometimes accompanied by surrounding edema, hemorrhage, or exudates. The primary risk associated with RAMs is the potential for leakage or rupture, which can cause vision loss due to macular edema, subretinal hemorrhage, or vitreous hemorrhage.
Symptoms of a RAM may include blurred vision, distorted vision (metamorphopsia), or sudden vision loss. Diagnosis is typically made through fundoscopic examination, fluorescein angiography (FA), and optical coherence tomography (OCT). FA can help visualize the aneurysm and assess for leakage, while OCT can evaluate retinal thickness and identify any associated edema or fluid accumulation.
Treatment options for RAMs depend on the severity of the condition and the presence of complications. Observation may be appropriate for small, asymptomatic aneurysms. Laser photocoagulation, anti-VEGF injections, or vitrectomy surgery may be considered for symptomatic RAMs with significant leakage, hemorrhage, or macular edema. Early detection and prompt management are crucial to prevent vision-threatening complications associated with retinal macroaneurysms.
Diagnostic Terms
Understanding diagnostic terms is crucial for navigating retinal health. Visual Acuity refers to the sharpness of vision, often measured using a Snellen chart. Refraction assesses how light bends as it enters the eye, identifying refractive errors like myopia or hyperopia.
Tonometry measures intraocular pressure, essential for glaucoma screening. Ophthalmoscopy allows direct visualization of the retina, optic disc, and blood vessels. Fundus Photography captures images of the retina for documentation and monitoring disease progression.
Fluorescein Angiography (FA) uses dye to visualize retinal blood vessels, detecting abnormalities like leakage or blockages. Optical Coherence Tomography (OCT) provides detailed cross-sectional images of the retina, aiding in the diagnosis of macular diseases and glaucoma. Electroretinography (ERG) measures the electrical activity of retinal cells, useful in diagnosing inherited retinal disorders.
Visual Field Testing assesses peripheral vision, detecting blind spots or visual field loss. Amsler Grid helps monitor for metamorphopsia (distorted vision), a symptom of macular degeneration. B-scan Ultrasonography uses sound waves to image the eye’s internal structures, especially when the view is obscured by cataracts or other opacities. These diagnostic tools are vital for comprehensive retinal evaluation and management.
Refraction of the Eye: Bending of Light
Refraction is the bending of light as it passes through different mediums, a crucial process for clear vision. The cornea and lens are the primary refractive structures in the eye. Light rays must focus precisely on the retina for sharp image formation.
Emmetropia describes the state where light focuses correctly on the retina, resulting in normal vision. Refractive errors occur when light doesn’t focus properly. Myopia (nearsightedness) happens when light focuses in front of the retina, causing blurry distance vision. Hyperopia (farsightedness) occurs when light focuses behind the retina, leading to blurry near vision.
Astigmatism results from an irregularly shaped cornea or lens, causing distorted vision at all distances. Refractive errors are corrected with eyeglasses, contact lenses, or refractive surgery. Diopters measure the refractive power of lenses needed for correction. The process of determining the refractive error is called a refraction, performed by an eye care professional.
Understanding refraction is essential for diagnosing and managing vision problems. Proper refraction ensures light focuses accurately on the retina, enabling clear and comfortable vision. Regular eye exams help detect and correct refractive errors, preserving optimal visual function throughout life.